- Get link
- X
- Other Apps
- Get link
- X
- Other Apps
Prior Authorization Request Form. Prior Authorization Correction Form.
Https Www Ahip Org Wp Content Uploads 2018 01 Joint News Release Prior Authorization Consensus Statement Pdf
AMA Update NCVHS Full Committee Meeting Expert Panel on Prior Authorization November 13 2019.

American health group prior authorization. Then select the Prior Authorization and Notification tool on your Link dashboard. FOR CROHNS DISEASE PATIENT MUST HAVE A DOCUMENTED FAILURE WITH AT. Director Administrative Simplification Initiatives.
Prior Authorization Criteria Health Alliance Plan_2018_HAPFB Date Effective. This approval process is called prior authorization. Online by using the Prior Authorization and Notification tool on Link.
Prior Authorization Medical Documentation Form. Prior authorization is a health plan cost-control process that requires providers to qualify for payment by obtaining approval before performing a service. Prior Authorization is a term used for select services eg homecare services items eg Durable Medical Equipment purchases over 500 and prescriptions for some injectable or infusion drugs eg Botox Soliris OxyContin that must be pre-approved by Health Partners Plans.
112018 Formulary ID 18297 V23 15 Other Criteria PRIOR TO RECEIVING BIOLOGIC THERAPY. As experience is gained these processes will be further refined to maximize efficiency and minimize care disruption for patients. AHA others collaborate to streamline prior authorization Jan 17 2018 - 0354 PM The AHA Americas Health Insurance Plans American Medical Association American Pharmacists Association Blue Cross Blue Shield Association and Medical Group Management Association today released a consensus statement outlining their shared commitment to improving the prior authorization.
It is overused costly inefficient opaque and responsible for patient care delays. In this section you will find the tools and resources you need to help manage your practices prior authorization and notification requirements with program specific information available for Cardiology Oncology Radiology Clinical Pharmacy and Specialty Drugs. Generally prior authorization for outpatient dialysis is met when.
And The treating provider has completed and signed a Monthly Certification of Emergency Medical Condition for the month in which outpatient dialysis services are received. Prior authorizations create administrative burdens for providers patients and payers the American Hospital Association AHA Americas Health Insurance Plans AHIP American Medical Association AMA American Pharmacists Association APhA Blue Cross Blue Shield Association BCBSA and Medical Group Management Association MGMA agreed. For more details and the CPT codes that require prior authorization please visit.
Get the latest resources and information and learn more about how the AMA is leading reforms around prior authorization. AMA and groups like the American Academy of Family Physicians have argued that payers need to improve the prior authorization process. Prior authorization requirements can lead to negative clinical outcomes.
This will help patients have access to safe timely and affordable care while reducing administrative burdens for both health care professionals hospitals and health insurance. FESP Monthly Certification of Emergency Medical Condition. FESP Initial Dialysis Case Creation Form.
The treating physician has submitted the completed and signed Initial Dialysis Case Creation Form to AHCCCS. For all mental health and substance use disorder benefits my group health plan requires prior authorization from the plans utilization reviewer that a treatment is medically necessary but the plan does not require such prior authorization for any medicalsurgical benefits. This group of health care leaders is committed to ongoing collaboration to improve the prior authorization process for health care professionals health insurance providers and most importantly patients.
Prior Authorizations Some services medicines or items need approval from Health Partners before you can get the service. In a statement released with the survey findings AMA charged. A prior authorization PA sometimes referred to as a pre-authorization is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine medical device or procedure.
Prior authorizations are sometimes referred to as preauthorizations or precertifications or. Press Releases May 14 2021. Prior authorization a utilization management UM process used by health insurance companies to determine coverage for a prescribed procedure service or medication is now becoming a mandatory requirement by the vast majority of large insurance companies.
FOR RHEUMATOID ARTHRITIS PATIENT MUST HAVE A DOCUMENTED FAILURE WITH AT LEAST ONE DMARD. WASHINGTON January 17 2018 Physicians pharmacists medical groups hospitals and health insurance providers are working together to improve prior authorization processes for patients medical treatments also known as pre-approval. Use the Prior Authorization Forms available under the Rates and Billing section for faxed PA requests including.
Were taking a number of steps to reform prior authorization this year. In a new tip sheet we explain that for health insurers providers and patients prior authorization is not only complex but also highly controversial. The prior-auth process itself goes by several names including preauthorization prior approval precertification prior notification prospective review and prior review.
As might be expected physicians suspect health insurers use prior.
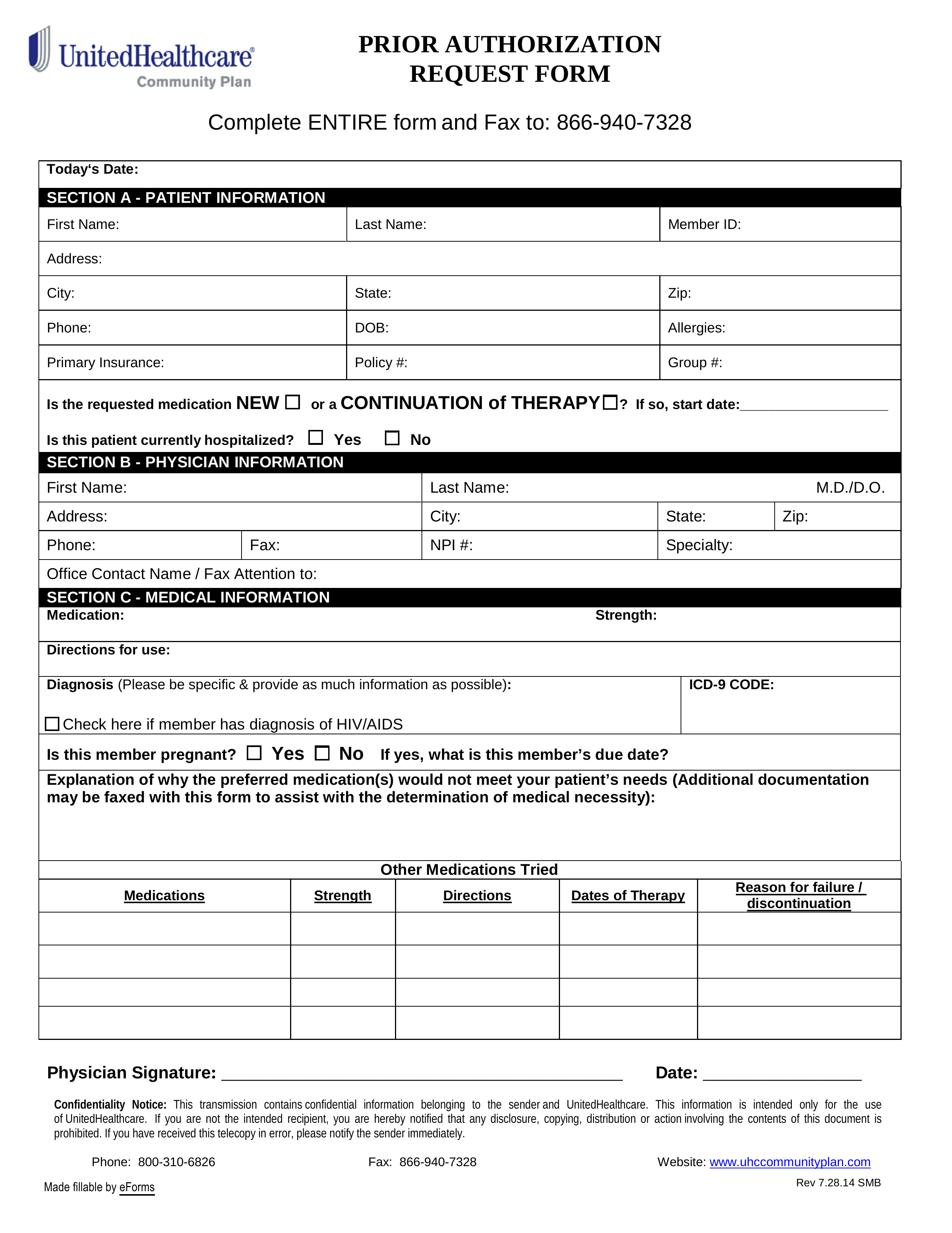 Free Unitedhealthcare Prior Rx Authorization Form Pdf Eforms
Free Unitedhealthcare Prior Rx Authorization Form Pdf Eforms
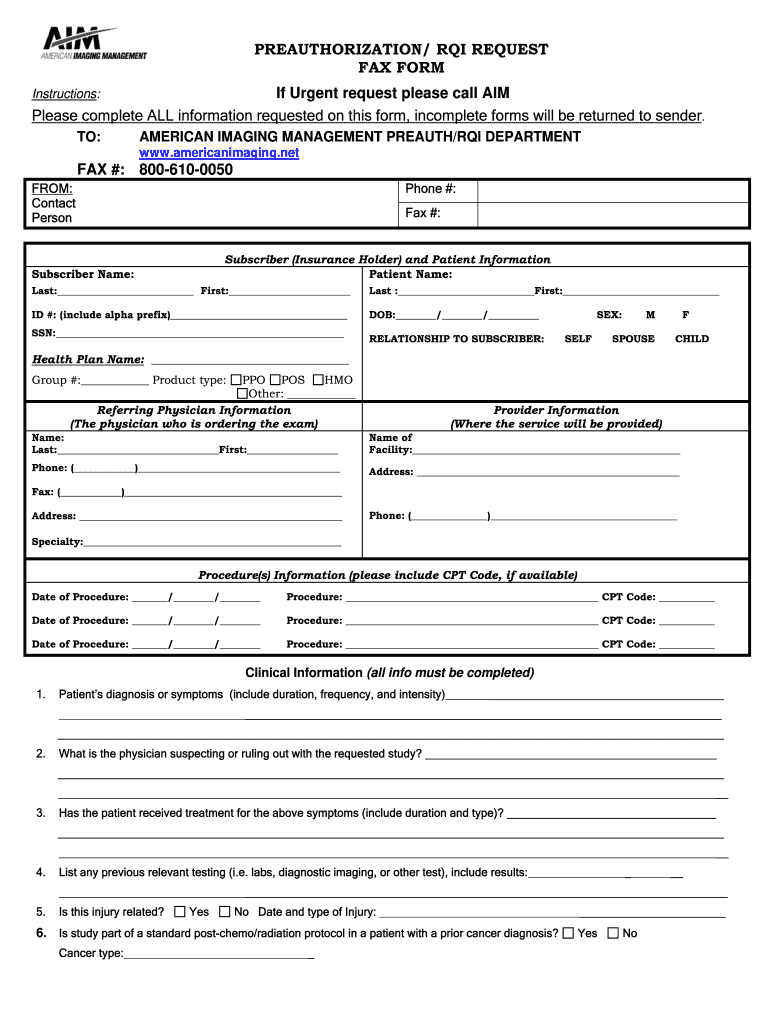 Aim Specialty Health Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Aim Specialty Health Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
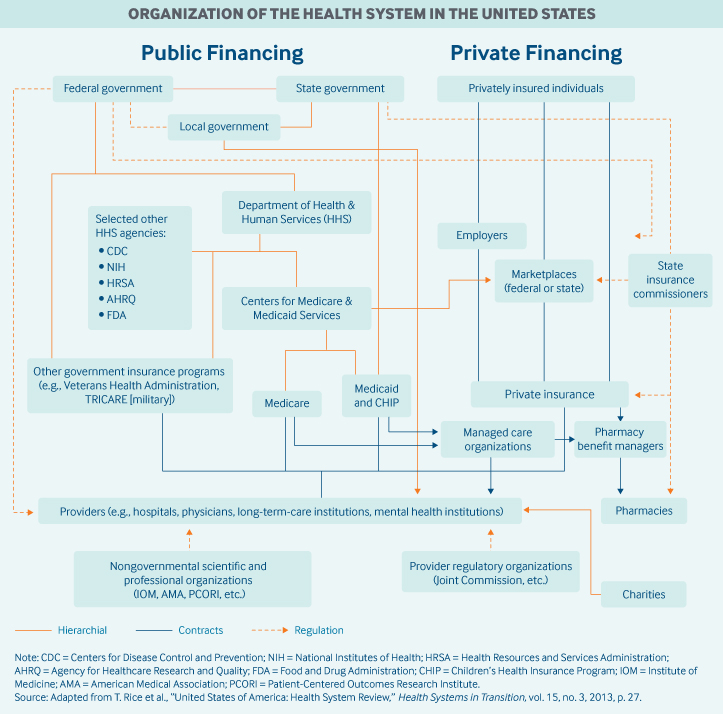 United States Commonwealth Fund
United States Commonwealth Fund
 Utilization Management American Health Holding
Utilization Management American Health Holding
Https Www Uhcprovider Com Content Dam Provider Docs Public Health Plans Medicare 2021 Qrg 2021 Qrg American Health Network Ohio Pdf
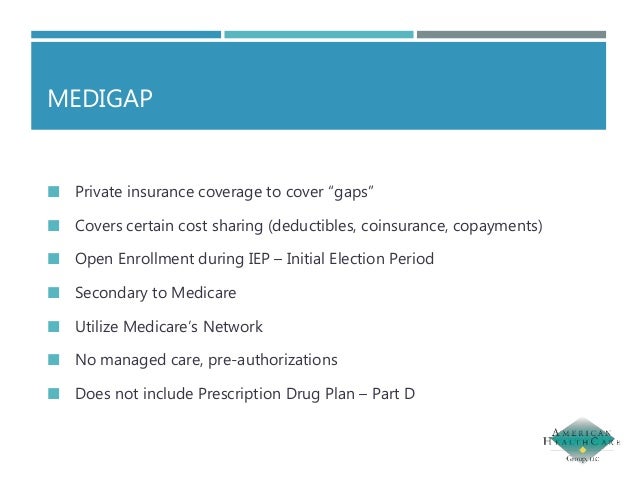 Medicare 101 Presentation From Erin Hart American Healthcare Group
Medicare 101 Presentation From Erin Hart American Healthcare Group
Https Kansashealthadvantage Com Wp Content Uploads 2020 H2392 Nsprvfaq20 C 20 20final 101019 Pdf
 Five Steps Of United Healthcare Procedure Prior Authorization Form To Get The Best Medical Assistance
Five Steps Of United Healthcare Procedure Prior Authorization Form To Get The Best Medical Assistance
 Prior Authorization Burden Continues To Rise Physicians Report
Prior Authorization Burden Continues To Rise Physicians Report
 Prior Authorization Needs Streamlining New Healthcare Coalition Including Ama Mgma Says Healthcare Finance News
Prior Authorization Needs Streamlining New Healthcare Coalition Including Ama Mgma Says Healthcare Finance News
 Under Prior Authorization Who Is Choosing Americans Medicines Stat
Under Prior Authorization Who Is Choosing Americans Medicines Stat
 Prior Authorization For Medical Services A Significant Pain Point For Providers And Practices Icd10monitor
Prior Authorization For Medical Services A Significant Pain Point For Providers And Practices Icd10monitor
Comments
Post a Comment