- Get link
- X
- Other Apps
- Get link
- X
- Other Apps
The proposed project will also evaluate by utilizing the. -Eliminate unnecessary services -Maximize savings to your health plan Healthcare services are evaluated for medical necessity appropriateness and efficiency of.
Utilization Management In Healthcare Smartsheet
Our Utilization Review Management Software allows the user to generate letters for the physician which can be sent out directly from within the system.
Utilization review tools. Within the information system and technology industry we have encountered the utilization of structured methods to minimize the crash of change and complexity the use of Computer Assisted Software Development India Engineering CASE tools to mechanize theSoftware Development India process the utilize of business reengineering methods to optimize organizational processes the employ of object. Individuals subject to a current Assisted Outpatient Treatment AOT court order. DWIHN Eligibility Service Review Tool.
Utilization Review UR for medical necessity has become highly complex with commercial products such as InterQual criteria becoming more stringent each calendar year. First and most importantly acute care review tools assume that subacute care and acute care are. B Intensity of ser- vice Severity of illness Discharge screens ISD C Managed Care Appropriateness Protocol MCAP and D Appropriate-.
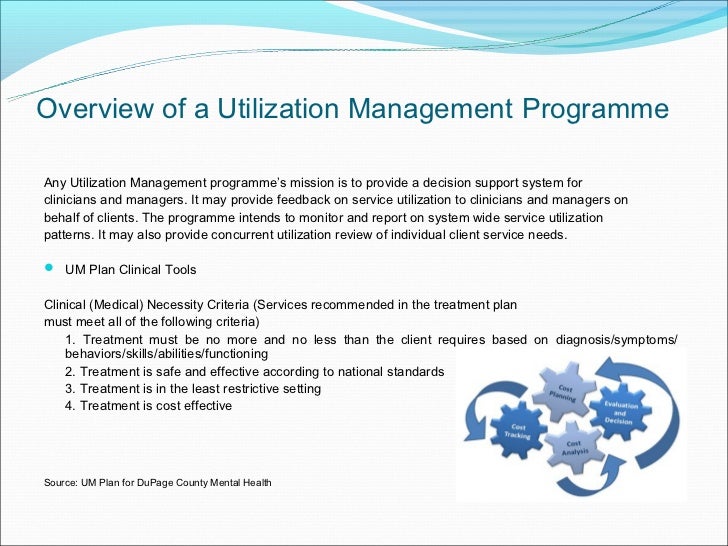
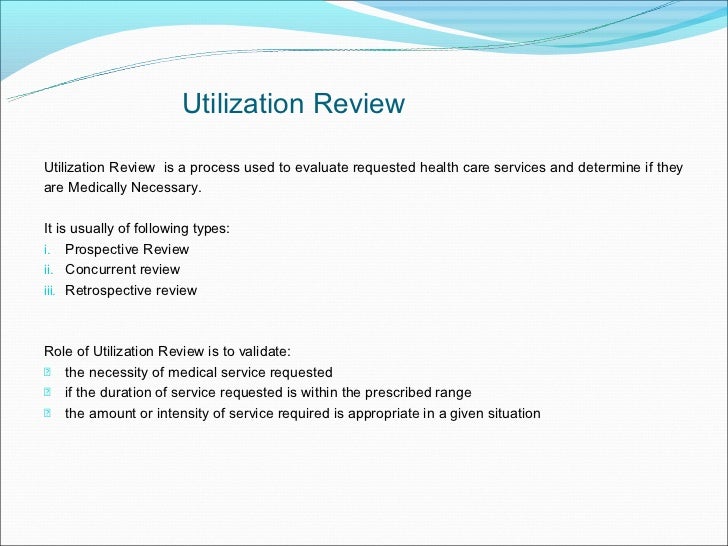
This process is called utilization review. Our pharmaceutical management procedures are integral in ensuring and promoting the utilization of the most clinically appropriate agent s to improve the health and well-being of our members. Utilization review is the process of making sure healthcare services are being used appropriately and efficiently which is a key component of a value-based approach to paying for health care.
This course gives nurses and Case Managers general working knowledge of what Utilization ManagementUtilization Review is including the definition process insurance principles and related laws. History of Utilization Review. UR generally refers to an insurance company or payer reviewing the services delivered by a healthcare providerthen determining whether those services fall under the coverage of the healthcare plan in question.
Utilization Management Tools. Is not on the PDL has an age edit exceeds established quantity limits is. 2021 Quality Monitoring Plan.
You can also edit a submitted prior authorization request in the tool. Utilization review UR is a process in which patient records are reviewed for accuracy and completion of treatment after the treatment is complete. Check prior authorization review status.
DWIHN Access Center Flow Chart. Simply put utilization review is the process of looking carefully at how healthcare benefits are being used. The goal of utilization review is to make sure patients get the care they need that its administered via proven methods provided by an appropriate healthcare provider and delivered in an appropriate.
-Ensure high quality care is delivered to those who medically need it. Utilization Review- A mechanism used by some insurers and employers to evaluate healthcare on the basis of appropriateness necessity and quality. UR a separate activity can be a part of UM specifically during retrospective review and can drive changes to the UM process.
To request an evaluation of a pharmaceutical that. A template is included below to help direct the review process The practitioner must supply the diagnosis the symptoms that cause difficulty in day-to-day functioning a proposed treatment plan. Sign in to the online prior authorization tool to get the status of a request.
Norman Kalant and colleagues conclude that utilization review tools are not valid to assess appropriateness of setting1We argue that this conclusion is not supported for several reasons. Utilization review for facility-based care is conducted over the telephone. Cian experts and 3 utilization review tools.
Telligens utilization management program is designed to. You can search for requests by reference number requesting provider or patient name. 51 Recommended Patient-related Triggers for Utilization Review of Acute Services To ensure clinically-appropriate and parity-compliant coverage the State recommends insurers only conduct utilization review for acute services inpatient or partial hospital programs for patients who meet the following clinical criteria.
Utilization management ensures services provided are medically necessary and provided at the appropriate and least costly level of care. The proposed project is an investigation of a community hospitals journey in converting to UR software and evaluating the outcomes after the implementation of the UR tool. Behavioral Health Utilization Management Review Policy.
Utilization review is a method used to match the patients clinical picture and care interventions to evidence-based criteria such as MCG care guidelines. Dual Eligible MHL Guidelines. Inpatient Acute Residential Psychiatric Utilization Review Services Admission Review Continued Stay Review Master Plan of Care Review Retrospective Review Peer Review Appeals Care Coordination Services.
Maximus provides online Level I Pre-Admission Screening and Resident Review PASRR screening online Level of Care utilization review for long term care populations and onsite independent PASRR Level II mental health and Level of Care evaluations. DWIHN Prior Authorized Service UM Chart Review Tool. Continued Stay Review- A type of review used to determine that each day of the hospital stay is necessary and that care is being rendered at the appropriate level.
Telligens Utilization Management program makes sure your members get the evidence-based medical care they need. This criteria helps to guide the utilization review nurse in determining the appropriate care setting for all levels of services across the arc of patient care. The practitioner may submit this information by telephone or by fax if it is routine outpatient treatment.
DWIHN Clinical Case Record Review Tool. The system provides integrated evidence-based guidelines that support CPT treatment codes.
Https Www Apg Org Wp Content Uploads 2018 10 Managed Care 101 Melanie Lite Matthews Pdf
 Pdf How Valid Are Utilization Review Tools In Assessing Appropriate Use Of Acute Care Beds
Pdf How Valid Are Utilization Review Tools In Assessing Appropriate Use Of Acute Care Beds
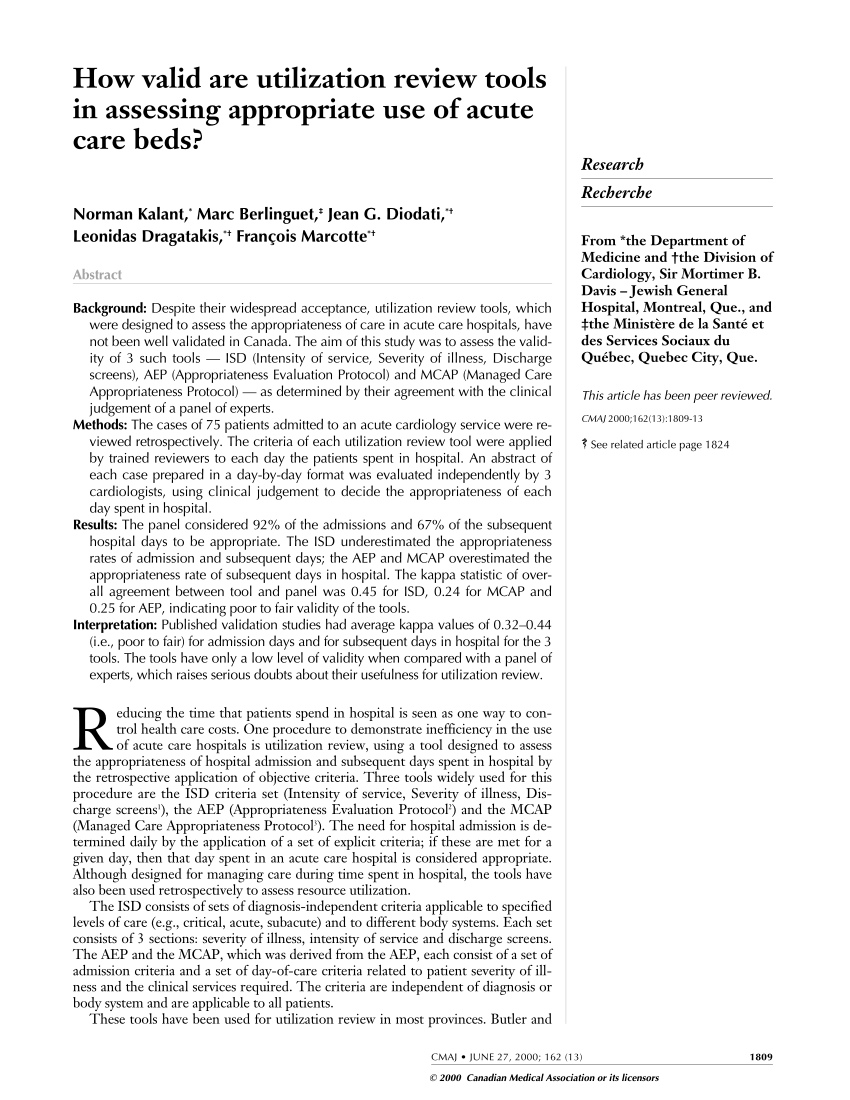
 Supermicro Systems Management Software Supermicro
Supermicro Systems Management Software Supermicro
 Pdf Validity Of Utilization Review Tools
Pdf Validity Of Utilization Review Tools
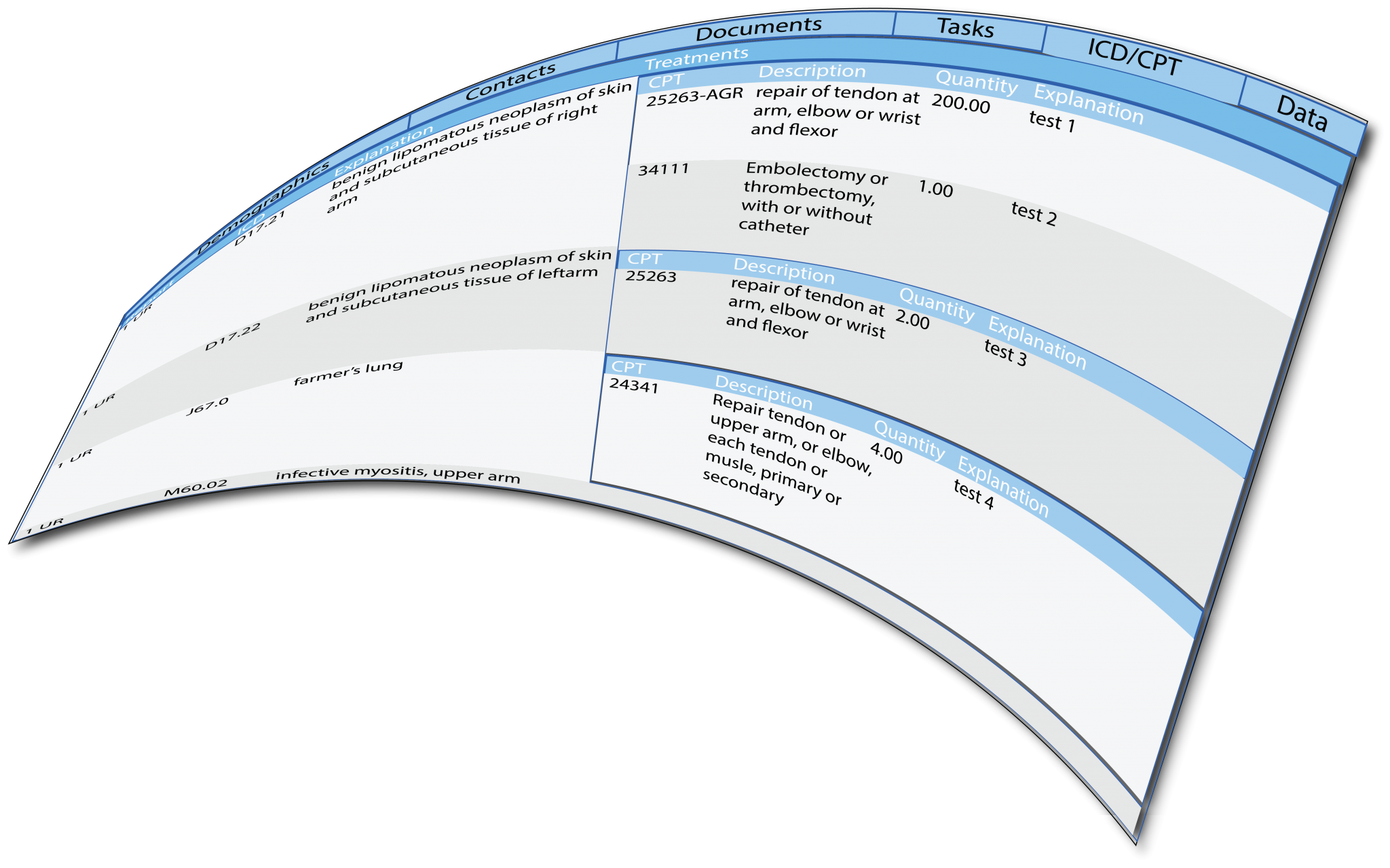 Utilization Review Software Datacare Request Free Demo
Utilization Review Software Datacare Request Free Demo
 Utilization Management Quality Improvement In Healthcare Study Com
Utilization Management Quality Improvement In Healthcare Study Com
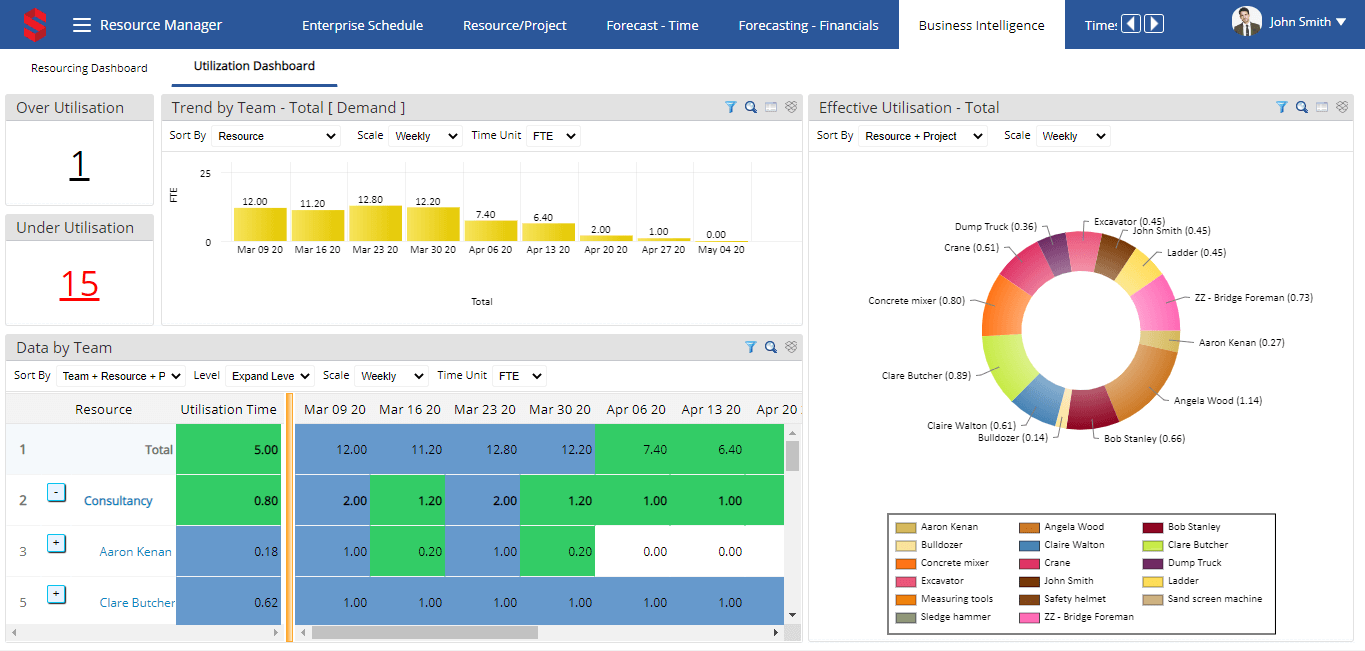 The 15 Best Resource Management Software Tools Of 2021 The Digital Project Manager
The 15 Best Resource Management Software Tools Of 2021 The Digital Project Manager
 Utilization Management Eqhealth Services
Utilization Management Eqhealth Services
Utilization Management In Healthcare Smartsheet
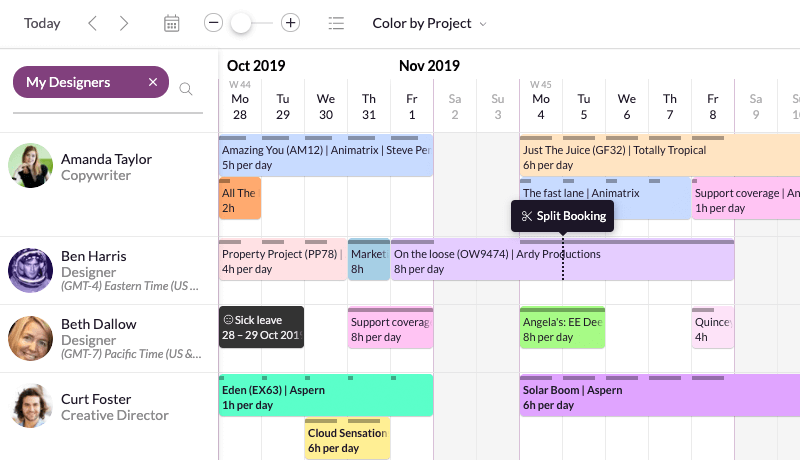 The 15 Best Resource Management Software Tools Of 2021 The Digital Project Manager
The 15 Best Resource Management Software Tools Of 2021 The Digital Project Manager
 Steps In The Act And Research Utilization Tools Translation Process Download Scientific Diagram
Steps In The Act And Research Utilization Tools Translation Process Download Scientific Diagram
Https Www Apg Org Wp Content Uploads 2018 10 Managed Care 101 Melanie Lite Matthews Pdf
Comments
Post a Comment